Brain fog and cognitive dysfunction are common symptoms experienced by people before, during and after migraine attacks that are associated with substantial burden.1,2 Indeed, after pain, difficulty thinking and worsening mental effort are rated by patients with migraine as the next most burdensome symptoms associated with migraine.2 This makes it important to understand what causes brain fog and how to manage it. During a plenary session at the 2024 American Headache Society (AHS) annual congress, Hsiangkuo Yuan, MD, PhD discussed current concepts in the mechanisms of brain fog in headache and other diseases and Elizabeth Seng, PhD, addressed objective and subjective cognitive symptoms during different phases of migraine attacks.
Defining ‘brain fog’
Brain fog is a subjective complaint that encompasses a variety of experiences when cognitive functions are not as sharp as usual.3 Patients experiencing brain fog variably associate it with traditional cognitive symptoms such as forgetfulness, difficulty concentrating, distractibility, inattentiveness, and but also with feeling groggy, fatigued, emotionally numb, depersonalization, and difficulty communicating (e.g., word finding difficulties).4
‘Brain fog’ is an umbrella term for subjective experiences of cognitive impairment
Possible causes of brain fog
Although there are several potential etiologies of brain fog, Dr. Yuan discussed three leading disease models of brain fog: long COVID, glymphatics, and microbiota. Persistent executive dysfunction affects up to one-quarter of individuals with long COVID5 and is worse in patients with more severe illness.6 Brain fog related to long COVID is thought to be a result of chronic neuroinflammation7 leading to neuronal and glial dysregulation, which alters neural circuits and cognitive function8 and has been associated with hypoperfusion in frontal and temporal lobes.9
Brain fog is a common complaint among people with long COVID
According to the glymphatic hypothesis, there exists a fluid circulation system between the cerebrospinal fluid (CSF) and the brain that is critical for bringing nutrients to the brain and eliminating waste products.10 A defective glymphatic system could therefore lead to toxin build-up in the brain; this has been demonstrated in individuals with dementia11 and other diseases associated with cognitive dysfunction.12 Dr. Yuan posited that impaired glymphatic function could lead to CSF congestion and thereby cognitive impairment, but this remains to be demonstrated in future studies.
Glymphatic dysfunction could be a contributor to brain fog
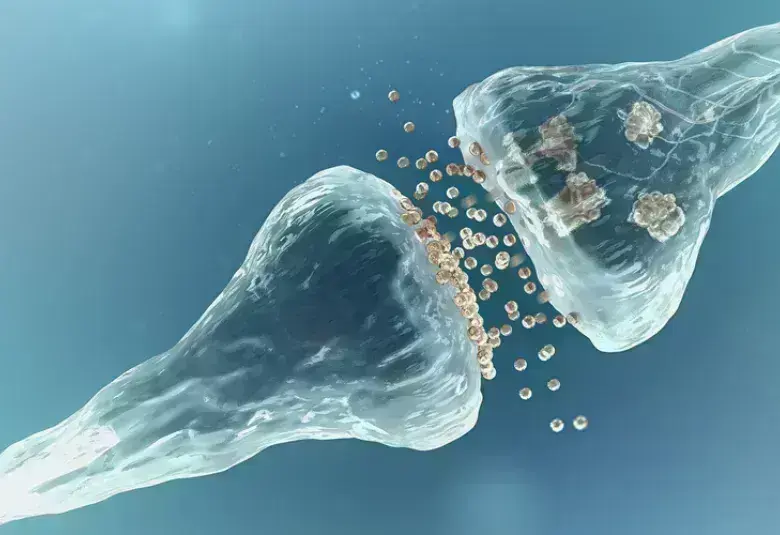
A third model relates to the bi-directional communication between the gut microbiota and the brain via the gut-brain axis.13 Metabolites from the gut microbiome including toxins that can damage myelin sheaths surrounding neurons could cross the blood-brain barrier and lead to cognitive dysfunction.13 In support of this hypothesis, studies have shown that the incidence of small intestinal bacterial overgrowth (SIBO) is higher in patients with brain fog14 and gut dysbiosis is more prevalent in people with migraine compared to healthy controls.15
The etiology of brain fog is an area of active research interest – leading hypotheses involve chronic neuroinflammation, glymphatic dysfunction, and dysbiosis
Cognitive symptoms across phases of migraine
While brain fog is a common complaint among patients with migraine, Dr. Seng highlighted differences in the prevalence of cognitive symptoms across different phases of migraine, suggesting that different mechanisms could be involved. Cognitive complaints are highest during the prodrome (90% of patients) and acute phases (88%), but they can persist during the postdrome and up to one-third of patients report persistent cognitive symptoms during interictal periods.1
Cognitive complaints are highest during the prodrome and headache phases
Different types of cognitive dysfunction are also reported across different phases of migraine. For example, ‘fogginess’ is more common during the prodrome and postdrome, difficulty concentrating is worst during the prodrome and headache phase, and memory problems are worst during the headache phase.1,16 According to Dr. Seng, this suggests that subjectively perceived cognitive symptoms such as brain fog could be predictors of an oncoming migraine attack.
Certain cognitive symptoms during the prodromal phase could signal an oncoming migraine attack
Cognitive exertion as a migraine trigger
Investigating cognitive impairment associated with migraine is challenging since migraine disincentivizes cognitive exertion. The term ‘cogniphobia’ was coined to describe this phenomenon of classic operant conditioning whereby patients with migraine avoid cognitive exertion for fear that it will cause a migraine attack.17 Patients with higher levels of cogniphobia have been found to show a weaker association between subjective and objective cognitive function,18 and Dr. Seng highlighted that this confounder should be considered when interpreting subjective reports of reduced cognitive functioning during migraine attacks.
Cogniphobia describes the avoidance of cognitive exertion out of fear that it will trigger a migraine attack
Future directions in brain fog and migraine
Objective cognitive declines have been observed during migraine attacks and they can be reversed with acute treatment. Other avenues of research should examine the associations between perceived and objective declines in cognitive function during migraine attacks, and the extent to which perceived and objective cognitive symptoms are characteristic of the prodrome and postdrome phases.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.