For nearly three decades, triptans were the only disease-specific class of medication for migraine. That all changed with the FDA's approval of the first calcitonin gene-related peptide (CGRP) inhibitor in 2018.1
Fast forward five years, Dr. David Dodick, a renowned headache expert from the Mayo Clinic, shared valuable insights about the advancements, efficacy, and safety considerations of CGRP inhibitors at the Canadian Pain Society (CPS) Annual Scientific Meeting 2023 in Banff, Alberta.
How do CGRP inhibitors work?
CGRP, a peptide found in sensory nerves throughout the body, plays a critical role in the mechanism of migraine. Upon the activation of trigeminal sensory afferents, CGRP is released, causing blood vessel dilation, neurogenic inflammation, and ultimately, headache.2
"CGRP is the most potent vasodilator in the body and is involved in various physiological reactions, both pathological and reparative."
CGRP inhibitors disrupt this process by blocking CGRP receptors, both peripherally, targeting A-Delta fibers at the nodes of Ranvier, and centrally, affecting the hypothalamus.3,4
"The hypothalamus is important as we believe migraine often originates there," Dr. Dodick emphasized. Imaging studies supporting this theory showed hypothalamic activation during the prodromal phase of migraine. Interestingly, patients who responded to CGRP inhibitors exhibited hypothalamic deactivation.5
CGRP inhibitors affect both peripheral and central nervous systems.
How effective are CGRP inhibitors?
"[As of now], the FDA has approved eight CGRP inhibitors, including four monoclonal antibodies and four gepants. The response rate to CGRP inhibitors is around 50% (between 40–62%) in patients with episodic migraine, and slightly less for those with chronic migraine," highlighted Dr. Dodick.
"Half of patients respond to CGRP inhibitors, based on the data from various clinical trials."
Despite similar response rates to second-generation anti-epileptic drugs used in the management of migraine, CGRP inhibitors are associated with a more tolerable adverse event profile.6 A large systematic review and meta-analysis that included 13 trials involving 7557 patients showed that patients on anti-CGRP monoclonal antibodies were 19.2 times more likely to benefit from these medications compared to those on second-generation anti-epileptic drugs.6 CGRP inhibitors also work faster and are less likely to be discontinued due to adverse events.7
However, while effective, CGRP inhibitors aren't disease-modifying. Yet, one-third of patients unresponsive to one CGRP inhibitor may still respond to another.8
"Patients are more likely to stay on CGRP inhibitors for a longer time. They won't discontinue them because of adverse events. And the longer you're able to stay on these drugs, the more effective they become over time."
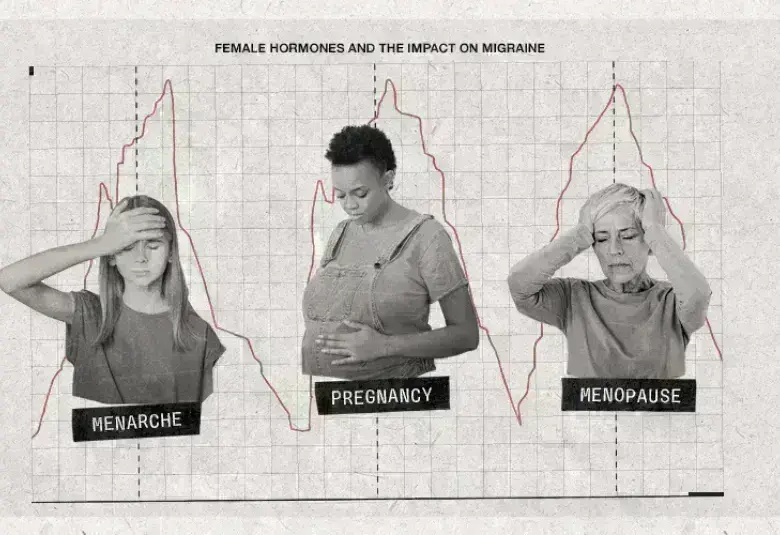
Who will respond well to the CGRP inhibitors?
Determining the likely responders to CGRP inhibitors is essential, particularly for women of reproductive age. Positive predictors of response include ictal allodynia, sensitivity/hypersensitivity, episodic migraine with lower headache frequency, unilateral pain or autonomic symptoms, and increased levels of salivary CGRP.9–12
In contrast, a less favorable response might be expected from those with psychiatric diseases, chronic migraine with medication overuse, failure of multiple preventive medications, obesity, and interictal allodynia.9–12
How safe are CGRP inhibitors?
When the first CGRP inhibitor was approved in 2018, constipation and injection site reactions were the only adverse events reported on the FDA label. However, additional adverse events have come to light in the last five years.
These include hypersensitivity, severe constipation, hypertension, Raynaud's phenomenon, hair loss, potential disruption in wound healing, and possible exacerbation of autoimmune diseases.11,13 Given this updated safety profile, clinicians need to closely monitor patients on CGRP inhibitors for these adverse events.
What does the future hold for migraine treatment?
Dr. Dodick expressed optimism about the future, highlighting the discovery of new neuronal targets for migraine treatment. Compounds such as protease-activated receptor 2 (PAR2) and pituitary adenylate cyclase-activating peptide (PACAP), which are currently undergoing phase two clinical trials.
Collectively, there are many exciting new possibilities in the near future for the field of migraine management.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.