Psychiatric disorders and diabetes are so common and inter-related that an entire chapter of the Diabetes Canada clinical practice guidelines are devoted to the subject. Dr. David Robinson, a psychiatrist in London, Ontario and lead author of the chapter, highlighted key aspects of the guidelines related to the burden, recognition, management, and monitoring of individuals with psychiatric disorders for incident or concurrent diabetes during a poster presentation at the annual Canadian Psychiatric Association (CPA) conference in Vancouver on October 20th, 2023.
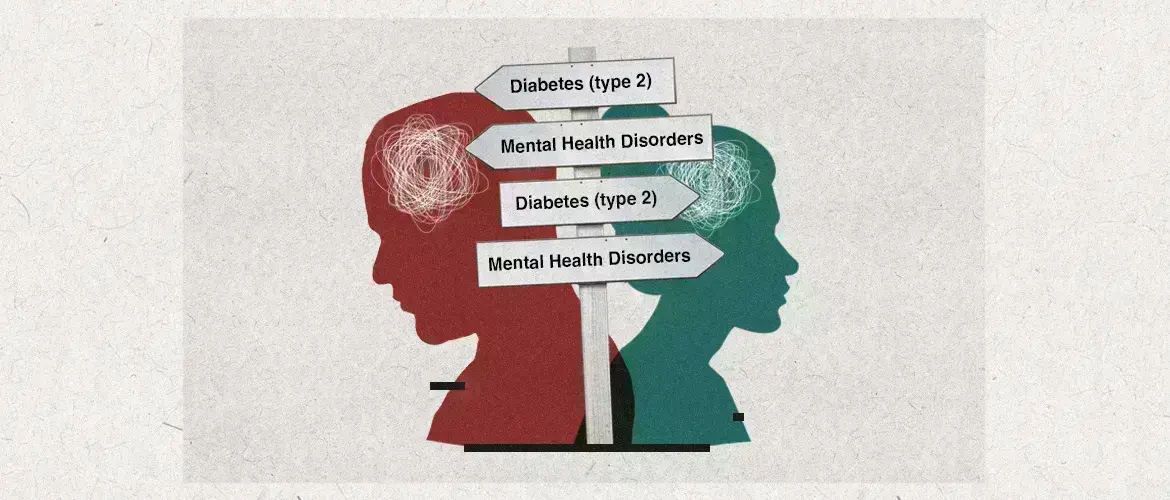
Complex bi-directional association between mental and metabolic health
A wide range of psychiatric disorders have been associated with an increased risk of diabetes, notably type 2 diabetes (T2D). While it is widely recognized that major depression, bipolar disorders, and schizophrenia spectrum disorders are associated with T2D, other disorders including substance use disorders, trauma, and eating disorders, neurodevelopmental disorders, personality disorders, neurocognitive disorders, gender dysphoria, and sleep-wake disorders also heighten the risk of T2D.
People with schizophrenia spectrum disorders have a 2- to 3-fold higher risk of diabetes
Likewise, diabetes increases the risk of various psychiatric disorders including depressive and anxiety disorders, substance use disorders, neurocognitive disorders, eating disorders, sexual dysfunctions and sleep-wake disorders.
People with diabetes have double the risk of major depression compared to the general population
The mechanisms behind these bi-directional associations are multifactorial and complex, and although they remain incompletely understood, they most likely involve intersecting biological, environmental, lifestyle and psychosocial factors. One important contributing factor underlying the association between diabetes risk and psychiatric disorders is disruptions in the sleep-wake cycle. Indeed, the elevated risk attributable to sleep-wake disorders is equivalent to traditional risk factors for T2D including overweight or obesity, family history, and physical inactivity.
Sleep-wake disruption is a significant risk factor for diabetes
Importantly, individuals with a psychiatric disorder and diabetes have significantly worse outcomes than individuals with diabetes alone, including higher diabetes-related morbidity and mortality, poorer quality of life and functioning, and increased healthcare costs. Conversely, the presence of diabetes increases the risk of rehospitalization in individuals with bipolar or psychotic disorders.
Psychotropic medications and diabetes risk
While some risk factors for diabetes are non-modifiable, there are other areas where clinicians can intervene to reduce the risk of diabetes in people with mental health disorders. Medication selection is one such factor that can impact diabetes risk, notably via their propensity for inducing weight gain. The Diabetes Canada guidelines offer a practical table categorizing psychotropic medications according to their weight gain potential, from unusual through to concerning.
When it comes to diabetes risk, not all psychotropic medications are equal
Antipsychotics as a class have been associated with metabolic concerns, but there is wide variability among individual agents, with third generation atypical antipsychotics having the lowest propensity for weight gain and metabolic dysregulation. Besides weight gain, antipsychotics may increase the risk of diabetes via direct effects on intracellular insulin signaling and b-cell responsiveness to glucose levels, as well as cholinergic pathway disruptions.
Third generation antipsychotics with lower propensity for weight gain are recommended by the Diabetes Canada guidelines
Practical recommendations for monitoring
The high burden of concurrent metabolic and mental health disorders underscores the importance of recognizing risk factors and acting on them as early as possible. To this end, the guidelines offer practical recommendations for baseline and follow-up monitoring of biometric and laboratory parameters as well as medical and family history.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.