Professor Joseph Coyle (Harvard Medical School, USA) presented his work spanning 50 years on the glutamatergic synapse and its role in the pathophysiology of schizophrenia in this APA Online 2022 session.
What is the NMDA receptor?
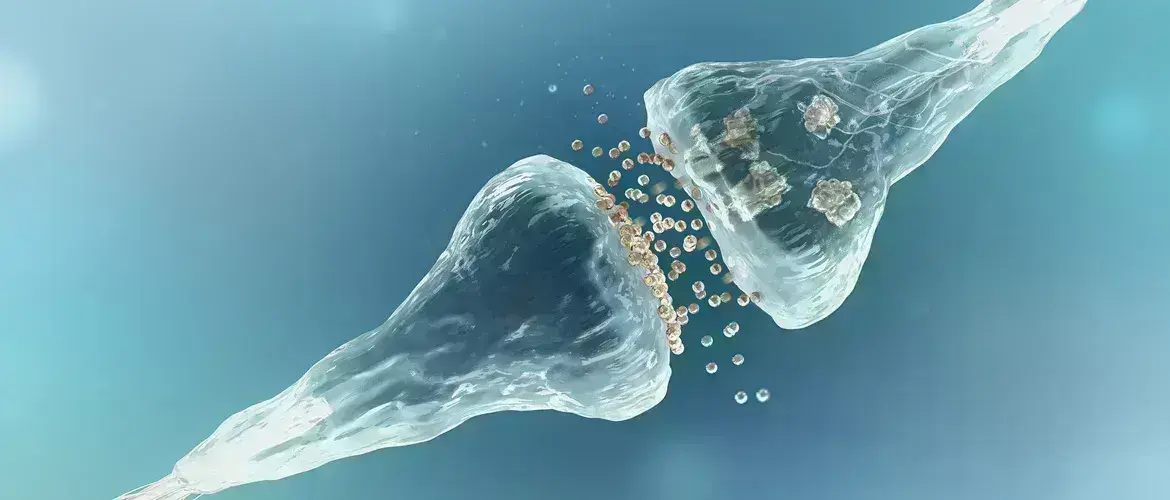
Professor Cole’s research has particularly focused on the N-methyl-D-aspartate receptor (NMDA-R)1. Glutamate is the main excitatory amino acid neurotransmitter in the brain, and the NMDA-R is one of the ionotropic receptors it activates2. The NMDA-R requires three events to open the channel: post-synaptic depolarization, binding of glutamate (at the glutamate site), and binding of a co-agonist (at the glycine modulatory site [GMS]). In the forebrain this is the amino acid D-serine, produced by the enzyme serine racemase. Calcium can then flow through the channel and induces expression of synaptic genes.
The NMDA-R is an important center of learning and memory
The NMDA-R has an important role in neuroplasticity, learning and memory. Ketamine and other dissociative anaesthetics are non-competitive antagonists, blocking the NMDA-R channel2.
Characterising the neuropathology
The 1970s saw a shift towards ‘biologic’ psychiatry with several significant publications in the schizophrenia field1. These included using computerised tomography to show correlation of increased cerebral ventricular size with cognitive impairment; demonstration of altered neurotransmitter activity; and proposal of the dopamine hypothesis.
Cortical atrophy severely affects the frontal cortex and temporal cortex, correlating with negative symptoms and cognitive impairment
Schizophrenia is characterised by positive symptoms, negative symptoms, and cognitive deficits, but it is only the latter two that predict disability. Specific brain structures are shrunken in schizophrenia with atrophy of the frontal cortex, temporal cortex, hippocampus and thalamus, resulting in 3-5% loss of volume1. There is neuronal atrophy and loss of dendritic spines3, resulting in a marked (approximately 30%) reduction in glutamatergic synapses1. Cortical atrophy is present at the onset of psychosis and progresses for at least a decade afterwards1. It is pervasive, but most severely affects the frontal cortex and temporal cortex, correlating with negative symptoms and cognitive impairment but not positive symptoms.
NMDA receptor dysfunction
NMDA receptor dysfunction is important in schizophrenia
Professor Coyle presented the glutamatergic dysfunction hypothesis of schizophrenia2, involving reductions in brain glutamate levels and glutamate carboxypeptidase II activity and increased levels of N-acetylaspartylglutamate. There is evidence that NMDA-R dysfunction is important in schizophrenia, demonstrated by elevated endogenous NMDA-R antagonists in the brain and cerebrospinal fluid (CSF) and reduced D-serine levels in CSF and serum2. Infusion of ketamine in normal volunteers replicates positive, negative, and cognitive symptoms of schizophrenia as well as some of the physiologic signs, such as hypofrontality and eye tracking2. Schizophrenia-like symptoms are also seen in autoimmune anti-NMDA-R encephalitis2.
Schizophrenia knockout mouse model
Prof Coyle described the serine racemase knockout mouse his group have developed as a model of NMDA-R dysfunction in schizophrenia4,5. These mice share many features with the cortical pathology of schizophrenia including cortical atrophy, reduced dendritic complexity and neuroplastic pathway function, cognitive impairment, and anhedonia. Some of these changes can be reversed by treating the mice with chronic D-serine5.
What about in humans?
Anti-tuberculosis drug, D-cycloserine, shows neuropsychological effects, including memory consolidation and fear extinction
In humans there is interest in the anti-tuberculosis drug D-cycloserine, a partial agonist at the NMDA-R GMS and alanine racemase inhibitor6. It crosses the blood brain barrier and has neuropsychological effects including memory consolidation and fear extinction. There is some evidence it can improve positive, negative, and cognitive symptoms in schizophrenia1.
The end of the beginning
Schizophrenia is a circuit disorder and not just a receptor disorder
Prof Coyle concluded that we are just at ‘the end of the beginning’ in understanding the biology of schizophrenia. He stressed the importance of remembering it is a circuit disorder and not just a receptor disorder. Future work will include expanding knowledge of genes associated with schizophrenia risk7, many of which affect glutamatergic neurotransmission, and crossover with risk factors for neurodevelopmental disorders and other conditions. D-cycloserine efficacy tends to reduce over time1 and other drugs are needed that work on this pathway.