Many lines of evidence over the past three years have suggested that COVID-19 infection may have negative impacts on mental health.1 While alarming, most of these studies are in hospitalized patients.
So what about people who have tested positive for COVID-19 but are well enough to avoid hospitalization? Would COVID-19 infection negatively impact their mental well-being?
A study from Ottawa Hospital Research Institute has an answer. The study, presented by Dr. Simon Hatcher at the 2022 CPA conference, found that non-hospitalized individuals who tested positive for COVID-19 did not have an increase in mental health disorders compared to those who tested negative.2
COVID-19 pandemic and mental health
As the COVID-19 pandemic spread, the number of studies on the psychological implications of COVID-19 infection increased.3
Despite the extensive research on mental health outcomes of the COVID-19 pandemic, “they all come to an inconsistent conclusion,” Dr. Hatcher said. “Some [studies] have said that there’s been a slight increase in mental health disorders, some said a big increase.”
“[The] jury is still out on what happens to your mental state after you get affected with COVID-19.”
In addition, the literature on the psychological implications of COVID-19 has a few limitations.
Most studies have been in hospitalized patients, even though 95% of COVID-positive individuals never get admitted to a hospital.4 “ Also, most of these studies don’t have a control group. So, you do not know what you are seeing is the effect of the pandemic or the virus,” Dr. Hatcher said. “And there is very little data on cognitive outcomes.”
Dr. Hatcher and his research team decided to conduct a study addressing these issues.
Study details
The study recruited participants who took a COVID-19 polymerase chain reaction (PCR) test between July 2020-Mar 2021 from a large community testing center in Ottawa Hospital. 162 participants with a positive test and 162 matched individuals with a negative test were enrolled in the study. Individuals who got hospitalized were excluded from the study.
The research team visited participants remotely once six months after their COVID-19 test result to complete study assessments.
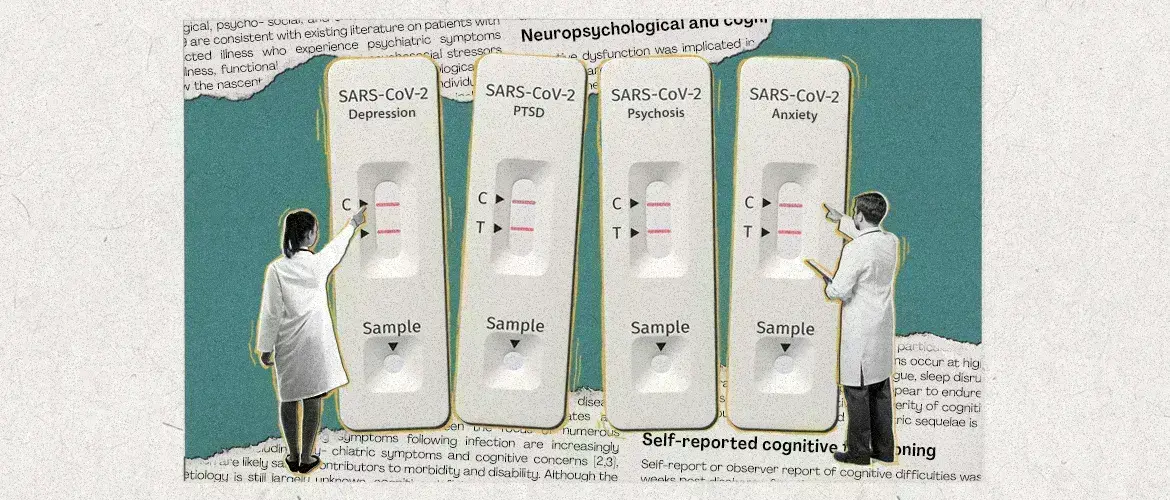
Researchers assessed participants for depression, anxiety, post-traumatic stress disorder, alcohol and substance use, and psychosis using a two-step assessment process. Before the study visit, participants completed self-reported questionnaires, which were used to decide about the need to do subsequent observer-rated assessments by the research team.
The cognitive performance of participants was also assessed using Mini-Addenbrooke’s Cognitive examination (M-ACE).
“Results were interesting,” Dr. Hatcher explained:
- Mental health outcomes did not differ between the two groups.
- Cognitive outcomes differ, but the difference was not statistically significant. 21.2% of participants in the COVID-positive group showed cognitive impairment (score < 25 on the M-ACE) compared to 13.8% in the COVID-negative group.
- In the COVID-positive participants, a psychiatric history, low income (less than $50,000), and a history of childhood trauma were predictors of depression and anxiety. However, low income was the only predictor of cognitive outcomes.
Non-hospitalized individuals who had a positive COVID-19 test did not have an increased rate of mental health disorders compared to those who tested negative, according to a Canadian study that followed 324 people for six months.
What’s the message of this study?
This study found no difference in mental health outcomes between individuals who tested positive vs those who tested negative for COVID-19. Moreover, the risk factors for mental health and cognitive outcomes were different between the two groups.
“So, it seems like, in non-hospitalized patients who tested positive for COVID-19, there is no evidence of an increase in mental health disorders compared to people who tested negative for COVID-19,” Dr. Hatcher said.
“What that means is any increase in mental health disorders during the pandemic is probably due to the effects of the pandemic, such as lockdown and not going to work,” Dr. Hatcher concluded.
“Increase in mental health disorders during the pandemic is probably due to the effects of the pandemic, such as lockdown and not going to work.”
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.